Subscribe to our newsletter!
© 2026 InsideOut
InsideOut acknowledges the tradition of custodianship and law of the Country on which the University of Sydney and Charles Perkins Centre campus stands. We pay our respects to those who have cared and continue to care for Country. We are committed to diversifying research and eliminating inequities and discrimination in healthcare. We welcome all people regardless of age, gender, race, size, sexuality, language, socioeconomic status, location or ability.
KEY POINTS
Anorexia nervosa is the deadliest of the mental disorders (3–6) and among the most expensive to treat in the public health system (1,7–10), yet eating disorders receive the lowest spend of mental health research funding, according to new research published in the [Lancet Regional Health](https://www.thelancet.com/journals/lanwpc/article/PIIS2666-6065(23)00104-9/fulltext) journal.
The analysis of funding allocations made by Australia’s three national medical research funding bodies (NHMRC, ARC and MRFF) over 13 years (2009-2021) reveals eating disorder research and treatment is consistently underfunded, contributing to protracted illness, a lack of treatment innovation, high death rates and significant health system costs. It is on every metric the most inequitably funded of the five major mental illness groups examined, having both the lowest actual dollar investment and the lowest per affected individual investment.
InsideOut Institute Director Associate Professor Sarah Maguire OAM says the lack of funding has “serious and long-standing impacts.”
“Despite a high mortality rate, increasing hospital presentations and attention from government, funding for eating disorders research hasn’t budged for more than a decade. This has led to a much smaller and poorly developed scientific community in this area, and a lack of innovation in treatments, which results in unnecessary illness and death,” said A/P Maguire of the University of Sydney.
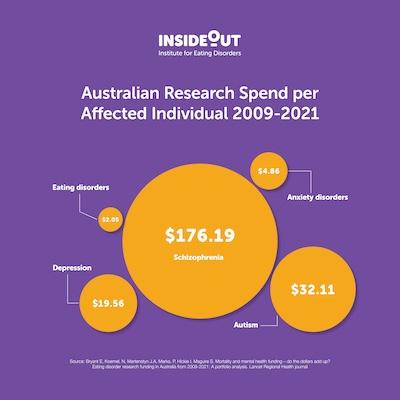
The analysis found a research spend of $2.05 per affected individual for eating disorders compared with $4.86 for anxiety disorders, $19.56 for depression, $32.11 for autism (which is currently funded under the mental health category) and $176.19 per affected individual for schizophrenia.
In actual dollar terms, both anxiety and depressive disorders get over seven times the investment in research received by eating disorders and the other two diagnostic groups analysed got double or more.
Burden of Disease (BoD) estimates are generally a primary consideration for medical research funding (12–15), but the analysis found that when it comes to eating disorders, there is a stark funding disparity relative to disease burden.
Study co-author and University of Sydney Researcher Emma Bryant says this mismatch could be due to stigma and a lack of robust epidemiological data.
“The lack of research investment means that what we know, and ask, about eating disorders in Australia is significantly less than other mental illnesses - we have no robust national epidemiological data, eating disorders have been excluded from national surveys, excluded from other routine mental health collections and mortality is poorly recorded. So, it’s very hard to get an accurate picture of who has an eating disorder, what kind of treatment they are getting and whether that treatment is effective”
“We believe official burden of disease figures for eating disorders are seriously underestimated, which has a flow on effect to the funding allocated,” said Ms. Bryant.
The analysis by Bryant, Maguire and the team of researchers from the University of Sydney’s InsideOut Institute for Eating Disorders, also found significant discrepancy between research funding dollars and disease burden associated with the mental and neurodevelopmental health in general.
Mental ill-health is responsible for up to 22% of total disease burden in established market economies (11). In Australia, mental ill-health causes the third highest all-age disability burden, and notably, the highest for young people and the health system cost of mental disorders doubles every seven years (16). But mental health receives less than 10% of total Australian public medical research funding (17,18).
A/Prof Maguire says eating disorders are getting a tiny portion of what is already too little an investment in the mental health of Australians.
“A systemic whole-of-government approach is needed to address inadequate investment in mental illness more broadly and particularly for illness groups such as eating disorders. Equitable, priority-driven allocation of medical research funding, commensurate with the true burden of illness, is essential to drive improvements in clinical care and the health of all Australians," said A/P Maguire.
Declaration: This work was in-part funded by the Australian Government Department of Health and the National Eating Disorder Research & Translation Strategy. The funder was not directly involved in informing the development of the current study.
Anyone needing support with eating disorders or body image issues is encouraged to contact:
References: