Last Reviewed: 01 Oct 2022
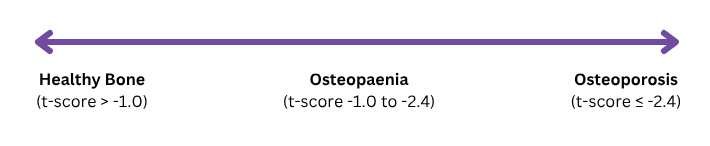
Bone health is on a spectrum, with healthy bone on one end, osteoporosis on the other, and osteopaenia (thinning of bone) in between. A Dual- Energy X-ray Absorptiometry (DEXA) scan of several bone sites in the body is used to determine Bone Mineral Density (BMD). The DEXA scan generates a Z-score or T-score of each bone site scanned, which is then used to determine whether an individual has healthy bone, osteopaenia or osteoporosis.
Osteoporosis is:
The systemic skeletal disease that is characterised by significant bone loss, deterioration of the microarchitectural structure of bone; causing compromised bone strength that predisposes the skeleton to fracture. (National Institute of Health, 2001)
Decreased bone mineral density (BMD) and strength is a common complication seen in individuals with eating disorders (Robinson et al 2019)
Factors that may put an individual at risk of decreased bone mineral density include:
Inadequate energy intake (Fazeli & Klibanski, 2018)
Low weight or loss of weight causing body composition changes and hormonal alterations (Misra & Klibanski, 2014; Misra et al, 2008)
Amenorrhoea (loss of menstruation) in females (Legroux & Cortet, 2019)
Low testosterone levels in males (Misra et al, 2008)
Pubertal delay or arrest (Gilsanz et al, 2011)
Family history of osteoporosis (Bijelic et al, 2019)
Smoking (AIHW, 2007)
Eating disorders may interfere with achieving peak bone mass during adolescence. Failure to achieve normal peak bone mass, or early loss of bone mass, may lead to premature development of osteoporosis. When women and girls are at a low body weight and/or have chronic caloric deprivation, they become hypo-oestrogenic (have low levels of the hormone oestrogen) (Fazeli & Klibanski, 2018). This is associated with low bone formation and high bone resorption, causing loss of bone (Bolton et al, 2005). When men and boys are at a low body weight, this causes low testosterone levels, which is correlated with low bone mineral density (Misra et al, 2008).
Bone mineral density was found to be reduced in patients with Anorexia Nervosa, where up to 92% of female patients had osteopaenia and 38% had osteoporosis (Grinspoon et al, 2000). A study found that male patients experienced significantly greater bone loss than females (Mehler et al, 2008). Weight is the most consistent predictor of BMD at all skeletal sites (Grinspoon et al, 2000), associating Anorexia Nervosa with low bone mineral density and an increased risk of fracture (Fazeli & Klibanski, 2018).
With regards to the effect of other eating disorders on BMD, individuals with persisting amenorrhoea, even if at a higher weight and with apparent minimal weight loss, remain at high risk for early development of osteopaenia and osteoporosis because of the effect of hormonal imbalance (Legroux & Cortet, 2019).
It is recommended that a medical team including an endocrinologist, dietitian, and physiotherapist are involved in the treatment plan for an individual with osteopaenia and/or osteoporosis. It is important to determine where on the bone health spectrum an individual’s bones lie, as this will inform the plan. It is possible to improve BMD in osteopaenia, however it is not possible in osteoporosis, but rather, the plan would be to prevent further deterioration and fractures.
The key to prevention, or minimising osteoporosis, is nutritional rehabilitation. This may include ensuring adequate energy balance, restoration of weight, and resumption of normal sex hormone metabolism (usually indicated by resumption of menses in females).
The following are recommendations to monitor bone health and prevent deterioration of bone mineral density:
Restoration of adequate nutritional status; including an increased energy intake and/or reduced energy expenditure, to ensure adequate energy balance to support hormone production, menses, and normal growth. (Legroux & Cortet, 2019; Misra & Klibanski, 2014; Hobart & Smucker, 2000)
Restoration of healthy weight and increased muscle mass. (Legroux & Cortet, 2019; Legroux-Gerot, et al, 2008; Misra & Klibanski, 2014; El Ghoch, et al, 2016; Bolton et al, 2005)
Ensure adequate intake of calcium and vitamin D containing foods.
Supplement intake of vitamin D and calcium if required (Drabkin, et al, 2017). However, calcium from food is always preferable.
Adequate sun exposure for vitamin D.
Referral to GP or Paediatrician for medical assessment of risk factors or conditions associated with osteoporosis (e.g., prolonged glucocorticoid therapy or thyroid medication, chronic liver and renal disease, or malabsorption disorders).
Whole body DEXA scan for females with eating disorders after 1 year of underweight (in children and young people), or earlier if they have bone pain or recurrent fractures, or after 2 years of underweight in adults, or earlier if they have bone pain or recurrent fractures. Do not repeat bone mineral density scans for people with anorexia nervosa more frequently than once per year unless they develop bone pain or recurrent fractures. (NICE, 2017)
Referral for assessment of hormonal status by an Endocrinologist or Paediatrician is recommended if there are signs of pubertal arrest, regression or slowed growth. The use of hormone therapy or bisphosphonates can then be considered, if appropriate (NICE, 2017).
The use of oestrogen and birth control is not recommended in the treatment of osteoporosis. (Legroux & Cortet, 2019)
If osteopaenia or osteoporosis is detected, reduce high impact physical activity and activities that that significantly increase the chance of falls and fractures (NICE, 2017).
If osteopaenia or osteoporosis is detected, consider referral to a physiotherapist who specialises in eating disorders, but only if the individual is medically stable and nutritional intake allows for increased energy expenditure. This should be thought about carefully, taking into consideration the individual's relationship with exercise and whether introduction of exercise may cause more harm (Drabkin, et al, 2017).
References
Australian Institute of Health and Welfare. (2007). Impairments and Disability Associated with Arthritis and Osteoporosis. Arthritis series no. 4. Cat. no. PHE 90. Canberra: AIHW, https://www.aihw.gov.au/getmedia/d34d2bdf-ac6d-40ee-99b1-c6979d4dd483/aposia.pdf.aspx?inline=true
Australian Institute of Health and Welfare. (2020). Osteoporosis. Cat. no. PHE 233. Canberra: AIHW, https://www.aihw.gov.au/reports/chronic-musculoskeletal-conditions/osteoporosis
Bijelic, R., Milicevic, S., & Balaban, J. (2019). ‘The Influence of Non-preventable Risk Factors on the Development of Osteoporosis in Postmenopausal Women’, Mater Sociomed, 31(1): 62–65. doi: 10.5455/msm.2019.31.62-65
Bolton, J. G. F., Patel, S., Lacey, J. H., & White, S. (2005). ‘A prospective Study of Changes in Bone Turnover and Bone Density Associated with Regaining Weight in Women with Anorexia Nervosa’, Osteoporosis International, 16, 1955-1962. doi: 10.1007/s00198-005-1972-7
Drabkin, A., Rothman, M. S., Wassenaar, E., Mascolo, M., & Mehler, P. S. (2017). ‘Assessment and Clinical Management of Bone Disease in Adults with Eating Disorders: A Review’, Journal of Eating Disorders, 5: 42. doi:10.1186/s40337-017-0172-0
El Ghoch, M., Gatti, D., Calugi, S., Viapiana, O., Bazzani, P. V., & Grave, R. D. (2016). ‘The Association Between Weight Gain/Restoration and Bone Mineral Density in Adolescents with Anorexia Nervosa: A Systematic Review’, Nutrients, 8(12), 769. doi: 10.3390/nu8120769
Fazeli, P. K., & Klibanski, A. (2018). ‘Effects of Anorexia Nervosa on Bone Metabolism’, Endocrine Reviews, 39(6), 895-910. doi: 10.1210/er.2018-00063
Gilsanz, V., Chalfant, J., Kalkwarf, H., Zemel, B., Lappe, J., Oberfield, S. E., Shepherd, J., Wren, T., & Winer, K. K.(2011). ‘Age at Onset of Puberty Predicts Bone Mass in Young Adulthood’, The Journal of Pediatrics, 158(1), 105. doi: 10.1016/j.jpeds.2010.06.054
Grinspoon, S., Thomas, E., Pitts, S., Gross, E., Mickley, D., Miller, K., Herzog, D., & Klibanski, A. (2000). ‘Prevalence and Predictive Factors for Regional Osteopaenia in Women with Anorexia Nervosa’, Annals of Internal Medicine, 133(10), 790-794. doi: 10.7326/0003-4819-133-10-200011210-00011
Hobart, J. A., & Smucker, D. R. (2000). ‘The Female Athlete Triad’, American Family Physician, 61(11), 3357-3364.
Legroux, I., & Cortet, B. (2019). ‘Factors Influencing Bone Loss in Anorexia Nervosa: Assessment and Therapeutic Options’, Rheumatic & Musculoskeletal Diseases, 5. doi:10.1136/rmdopen-2019-001009
Legroux-Gerot, I., Vignau, J., Collier, F., & Cortet, B. (2008). ‘Factors Influencing Changes in Bone Mineral Density in Patients with Anorexia Nervosa-Related Osteoporosis: The Effect of Hormone Replacement Therapy’, Calcified Tissue International, 83, 315-323. doi: 10.1007/s00223-008-9173-y
Mehler, P.S., Sabel, A.L., Watson, T., Andersen, A.E. (2008). ‘High Risk of Osteoporosis in Male Patients with Eating Disorders’, International Journal of Eating Disorders, 41:7 666–672. doi:10.1002/eat.20554
Misra, M., & Klibanski, A. (2014). ‘Anorexia Nervosa and Bone’, Journal of Endocrinology, 221(3), R163-R176. doi: 10.1530/JOE-14-0039
Misra, M., Katzman, D. K., Cord, J., Manning, S. J., Mendes, N., Herzog, D. B., Miller, K. K., & Klibanski, A. (2008). ‘Bone Metabolism in Adolescent Boys with Anorexia Nervosa’, Journal of Clinical Endocrinology and Metabolism, 93, 3029– 3036. doi:10.1210/jc.2008-0170
National Institute of Health (NIH) Consensus Development Panel on Osteoporosis Prevention, Diagnosis, and Therapy. (2001). Osteoporosis Prevention, Diagnosis, and Therapy. JAMA. 285, 785–95
National Institute for Health and Care Excellence. (2017). ‘Eating Disorders’: Recognition and Treatment’ (NICE Guidelines NG69). NICE.
National Institute of Health (NIH) Consensus Development Panel on Osteoporosis Prevention, Diagnosis, and Therapy. (2001). Osteoporosis Prevention, Diagnosis, and Therapy. JAMA. 285, 785-95
Robinson, L., Aldridge, V.K., Clark, E.M., Misra, M., Micali, N. (2019), ‘Bone health in adult women with ED: A longitudinal community-based study’, Journal of psychosomatic research, 116, 115–122. doi: 10.1016/j.jpsychores.2018.12.005
On this page:
Subscribe to our newsletter!
© 2026 InsideOut
InsideOut acknowledges the tradition of custodianship and law of the Country on which the University of Sydney and Charles Perkins Centre campus stands. We pay our respects to those who have cared and continue to care for Country. We are committed to diversifying research and eliminating inequities and discrimination in healthcare. We welcome all people regardless of age, gender, race, size, sexuality, language, socioeconomic status, location or ability.