An estimated 1 million people in Australia are living with an eating disorder, but only around 1 in 5 of them receive care in the health system. Of those that do get treatment, research suggests that only a small portion will receive evidence-based care. Statistics such as these are alarming as we know that recovery rates are improved with earlier intervention and shorter duration of illness.
Reducing this treatment gap – and ensuring people with eating disorders get the help that they urgently need where and when they need it – will require concerted effort, investment and innovation across several domains, particularly at the point of care.
And that is precisely what the Clinical Decision Support Tool for GPs is designed to do.
What exactly is the Clinical Decision Support Tool?
The Clinical Decision Support Tool is a digital tool for GPs that will help them in screening and care planning for people with eating disorders at any point in their presentation.
A key feature of the program is that it uses a diagnostic algorithm to walk GPs through the indicators of an eating disorder, in real time, to provide GPs with all the information they need to make appropriate diagnoses, and to facilitate speedy identification of symptoms.
It further provides GPs streamlined access to the evidence base on all things from diagnosis to gold-standard treatments. Importantly, the program will also provide resources and advice to support effective care planning and will help GPs link clients to treatment providers. The Clinical Decision Support Tool makes all of this vital information easily accessible at the point of care (or at any time!), and in this way, it is designed to be a timesaving and easy-to-navigate tool for busy GPs.
The program aims to be particularly effective in helping GPs to detect and intervene early in the illness course. That is, when people present to the GP with emergent symptoms. This is vital because we know that early intervention can improve outcomes for people with eating disorders, but they can be hard to identify, and many people fall through the cracks.
Alongside the Clinical Decision Support Tool is the Practice Management Toolkit. This comprehensive resource includes templates (i.e. eating disorder care plan templates), factsheets, guidelines, links to further learning, and other resources, which are needed to best support a whole of practice approach to people with eating disorders. It also includes resources that can be helpful for the person with an eating disorder and their family. This Practice Management Toolkit is designed to be uploaded onto GPs practice software and easily integrated into daily practice.
It is hoped that the Clinical Decision Support Tool will ultimately make it easier for GPs to open up a conversation with people deemed to be at risk, and more easily navigate pathways to evidence-based treatment.
How will this help GPs?
Dr Karen Spielman is part of the co-design team and a GP advisor on the project. She specialises in eating disorders and has cared for people with eating disorders for around 20 years. As well as being a director of a small mixed billing General Practice in Sydney and an active member of the Australian Society for Psychological Medicine, she was until recently lead GP at headspace Bondi Junction. She is also providing GP input to some other exciting research projects with InsideOut.
She says this tool is urgently needed.
“GPs are now more often in the position of needing to manage diverse eating disorder presentations in the community due to both the increasing prevalence and the difficulty accessing other support services,” she says.
Dr Spielman says that when it comes to early detection and improving pathways to care, this project is an important piece of the puzzle.
“GPs are perfectly placed to support patients and their families and if better resourced will be able to make impactful contributions to the service provider landscape by both providing some treatments and improving navigation of the system.”
“It is my hope that GPs wherever they are across the country will make use of the tool in their daily practices and that it is useful for those who don’t know a lot about the area all the way to those who have a keen interest,” Dr Spielman says.
“This will bring doctors to evidence in a really simple way, providing a one-stop shop for GPs when it comes to helping people with eating disorders.”
“It will give them support and encouragement, so that they can have therapeutic conversations with people who may be at risk, and be effective intervening early.”
The development process
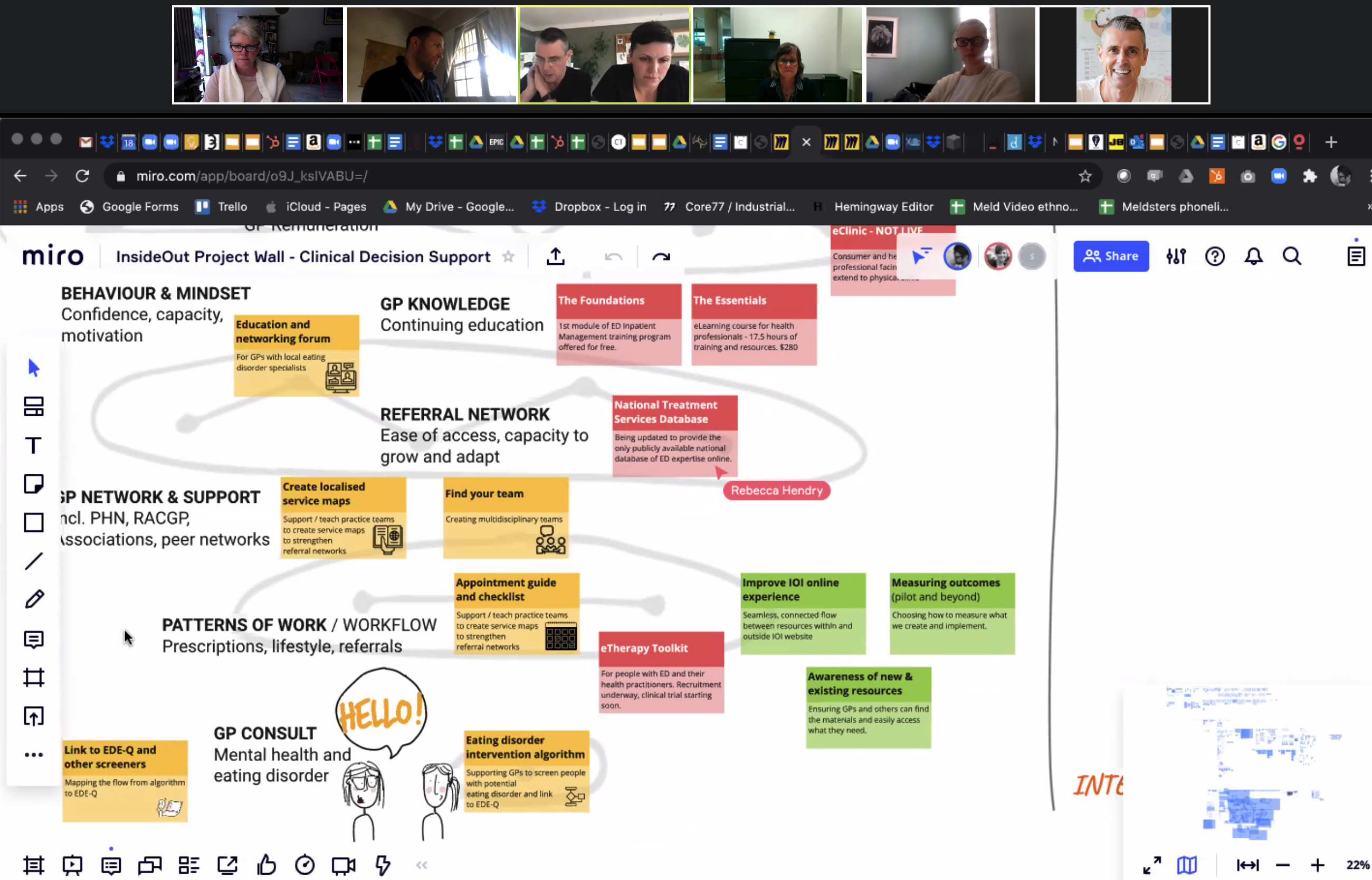
The Clinical Decision Support Tool has been co-designed every step of the way with extensive collaboration involving a raft of GPs, a range of eating disorder clinical experts, people with a lived experience of eating disorder and carers.
For the initial process analysis phase, InsideOut engaged Meld Studios to conduct a human-centred participatory research design approach. We asked GPs and people with lived experience (including patients and families) to share the things they felt were important for us to hear about in relation to help seeking, accessing treatment and talking about eating issues with a GP.
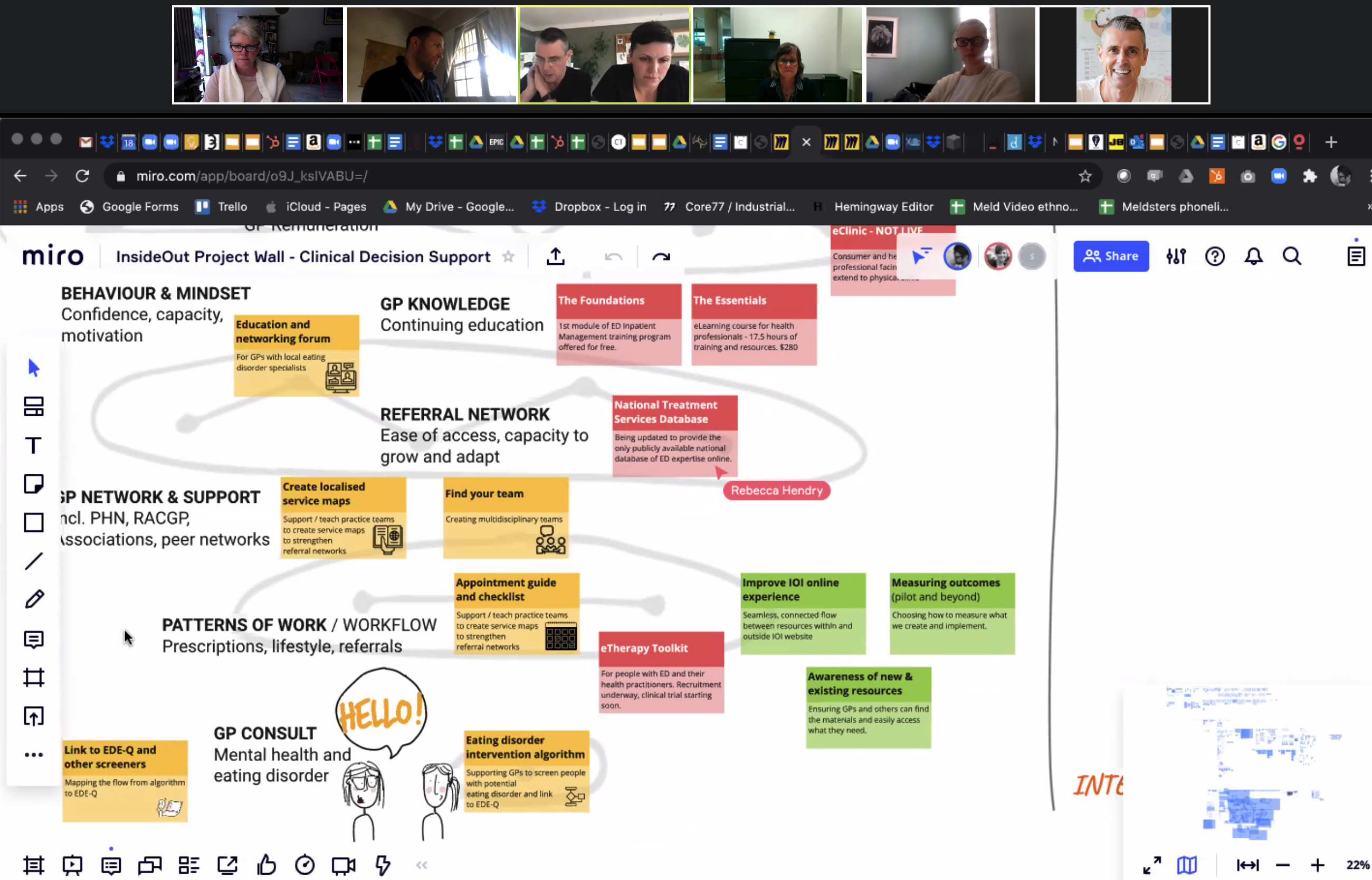
We also spoke to GPs about the kind of information they wanted that would be helpful to them, and what kind of resources they would and wouldn't use. We visited them in their practices and had a number of co-design workshops where we all came together – including with specialist ED clinicians – to come up with a framework.
These incredibly involved workshops helped to pinpoint what and how a digital tool could best support GPs and improve the patient experience and, ultimately, improve outcomes for people with eating disorders.
The design and development phase used an agile process, where every element of the Hub and support tool has been developed using an iterative process with end users (i.e. GPs). Once a part of the program was made, it would then be tested by a group of GPs to make sure it worked and that it was doing what they would like it to do. Then, the program was modified according to their feedback and trialed again – until the end product was perfected.
When will it be ready?
The design of the GP Hub and Clinical Decision Support Tool is now complete, and the digital build is underway. It is due for completion by the first half of 2022 when it will be ready for national roll-out and evaluation.
This project is funded by the Australian Government Department of Health and is one part of the Translation of Eating Disorder Evidence into Clinical Practice Grant, awarded to InsideOut in 2018. It is one of a number of projects funded by this grant, including the recently launched Australian Eating Disorders Research and Translation Strategy.